Mouthwash
Oral diseases need to be prevented through meticulous oral care as they cause discomfort due to bad breath and even tooth loss in severe cases. Among oral diseases, dental caries and periodontal disease are the most common, occurring in over 75% of adults [1]. Dental caries is an infectious disease accompanied by destruction, commonly occurring in all age groups, from children to the elderly, with the typical causative agent being Streptococcus mutans (S. mutans). Generally, S. mutans is most important for early biofilm formation and is known to cause dental caries through the process of adhering to tooth surfaces, proliferating, and producing acid [2]. The main causative agents are anaerobic bacteria such as Filamentous and Spirochetas, causing inflammation of connective tissue, loss of periodontal ligaments, and bone resorption in the tooth socket. To prevent and treat dental caries and periodontal diseases, the number of bacteria must be reduced and eliminated by preventing bacterial invasion [3]. To remove bacteria, mechanical tooth brushing, interdental brushing, and mouth rinsing are used as methods of mechanical plaque control, but if used incorrectly, irreversible damage to oral tissues can occur. Moreover, it is difficult for ordinary people to effectively remove bacteria from hard-to-reach areas using these methods, so instead, chemical plaque control methods can be used [4]. Among the existing chemical plaque control methods, mouth rinsing is currently the most widely used, and its use tends to increase due to its ease of use and portability of mouthwash bottles [5]. Chemical plaque control agents include Chlorhexidine (CHX) [6], Listerine® [7], fluoride [8], and mildly acidic hypochlorous acid (HOCL) [9]. In particular, CHX is the most commonly used mouthwash in dentistry because it is known to be the most effective agent against dental plaque [10].
Recently, the use of mouthwashes containing chemical components with antibacterial effects has been increasing [11]. Mouthwash is very useful for oral care in infants, those undergoing orthodontic treatment, the disabled, or the elderly due to its antibacterial effect in liquid form [12]. The effectiveness of mouthwash as a complementary means of removing dental plaque has been clinically proven and the number of users is increasing [13]. Moreover, it has been reported that when used to treat periodontitis or for maintenance after periodontal treatment, it can increase the success rate of periodontal treatment because it prevents the formation of dental plaque [14]. Ferguson also mentioned that the use of mouthwash helps reduce dry mouth when applied to patients with dry mouth [15]. There are many studies on the superior efficacy of HOCl mouthwash. Please refer to the study by Yu-rin Kim and Seoul-Hee Nam, funded by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning
Purpose of the study: To compare the preventive effects of HOCl mouthwash and chlorhexidine (CHX) mouthwash as plaque control agents for oral diseases. This study was conducted on three groups: 1 group rinsed with 0.005% CHX, 1 group rinsed with mildly acidic HOCl, and 1 group rinsed with saline. Patients were instructed to rinse with 15 ml of each mouthwash for 1 minute, and then spit for 1 minute to remove any remaining mouthwash. Halitosis (BB Checker), O’Leary index (plaque assessment), cariogenic activity (Snyder test measuring bacterial acid production rate), bacterial species, and motility were then measured.
Results: There was no significant difference between the saline and CHX groups, but there was a significant reduction in the HOCl group. The O’Leary index, Snyder test, bacterial motility, and Filamentous were reduced more effectively in the HOCl group compared to the CHX group, showing significant differences in all parameters.
Halitosis: In all three groups, the normal value was shown to be 0-50 BBV. There was no significant difference in halitosis between the saline and CHX groups, and halitosis values were found to be significantly lower in the HOCl group.
Comparison of O’Leary plaque index: The O’Leary index was high in the saline group, and this index was lower in the HOCl group compared to the CHX group. In quantitative results, there was a clear significant difference between the three groups, and the most effective reduction was shown in the HOCl group.

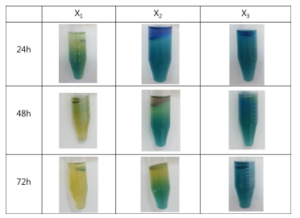
X1: brine X2: CHX X3: HOCl
Comparison of cariogenic activity using the Snyder test: In the comparison of cariogenic activity, there was a significant difference between the three groups (p < 0.05). In the Snyder test for the saline rinse group, the subjects’ teeth turned yellow after 24 hours of incubation, indicating a high risk; the teeth of subjects in the CHX rinse group turned yellow after 48 hours of incubation, indicating moderate to low activity; and the teeth of subjects in the HOCl rinse group did not show any color change throughout the 72-hour incubation period, indicating no activity, which is the safest condition in terms of cariogenic activity.
Periodontitis: In the HOCl mouthwash group, bacterial movement was significantly reduced. Specifically, there was a marked decrease in S. mutans and a significant reduction in Filamentous and Spirochetas, bacteria that cause periodontal diseases. There was a significant reduction in bacterial activity, especially filamentous bacterial activity, in the HOCl mouthwash group compared to the CHX mouthwash group.

Based on this research, CHX, which is currently widely used in dentistry, can be considered inconvenient to use due to its strong taste and smell, and there have been many reports of adverse effects on the oral cavity (tooth staining, gum discoloration) when used long-term. Therefore, if harmless HOCl with broad disinfecting abilities is used as a substitute for CHX, oral care will achieve safety and efficacy: preventing oral diseases, effectively caring for teeth by controlling dental plaque, reducing cariogenic activity, and decreasing bacterial acid production.

MiraChlor Mouthwash
- Eliminates bad breath
- Prevents plaque buildup
- Promotes healing of mouth sores
References:
-
- Ministry of Health and Welfare: 2012 Korean National oral health survey: III summary report. Ministry Health Welfare Seoul 2013.
- Hamada N, Takehara T. Virulence factors of Streptococcus mutans and dental caries prevention. J Dent Re. 1984; 63: 407-411.
- Slot J. Subgingival microflora and periodontal disease. J Clin Periodontol 1979; 6: 351-382.
- Jain Y. A comparison of the efficacy of powered and manual toothbrushes in controlling plaque and gingivitis: a clinical study. Clin Cosmet Investing Dent 2013; 27: 3-9.
- Ciancio SG. Agents for the management of plaque and gingivitis. J Dent Res 1992; 71: 1450-1454.
- Brecx MC, Liechti T, Widmer J, Gehr P, Lang NP. Histological and clinical parameters of human gingiva following 3 weeks of chemical (chlorhexidine) or mechanical plaque control. J Clin Periodontol 1989; 16: 150-155.
- Whitaker EJ, Pham K, Feik D, Rams TE, Barnett ML, Pan P. Effect of an essential oil-containing antiseptic mouthrinse on induction of platelet aggregation by oral bacteria in vitro. J Clin Periodontol 2000; 27: 370-373.
- Paraskevas S, Danser MM, Timmerman MF, Van der Velden U, Van der Weijden GA. Effect of a combination of amine/stannous fluoride dentifrice and mouthrinse in periodontal maintenance patients. J Clin Periodontol 2004; 31: 177-183.
- Ito K, Nishida T, Murai S. Inhibitory effects of acid water repared by an electrolysis apparatus on early plaque formation on specimens of dentine. J Clin Periodontol 1996; 23: 471-476.
- Lang NP, MC Brecx. Chlorhexidine digluconateab agent for chemical plaque control and prevention of gingival inflammation. J Periodontol Res 1986; 16: 74-89.11.Wade W. New approaches to the control of plaque are now being developed introduction. J Dent 2010; 38:
- Hua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochr Datab Syst Rev 2016; 25; 10: 008367.
- Ciancio SG. Agents for the management of plaque and gingivitis. J Dent Res 1992; 71: 1450-1454.
- Van Der Weijden FA, Van Der Sluijs E, Ciancio SG. Can chemical mouthwash agents achieve plaque/gingivitis control? Dent Clin North Am 2015; 59: 799-829.
- Furguson MM, Hayes P, Highton J, Jones DS, Macfadyen EE, Palmer DG. Pilocarpine oral solution. Letters 1991;251


